A major national effort to strengthen primary medical care has shown improvements in care delivery for Medicare patients two years into the initiative, according to a Mathematica Policy Research study that is detailed in an article in the New England Journal of Medicineand in a new report (with appendix).
The four-year Comprehensive Primary Care (CPC) initiative, launched in 2012, is one of the largest efforts by the Centers for Medicare & Medicaid Services (CMS) to improve primary care. Medicare is partnering with commercial payers and state Medicaid agencies to provide funding and support to nearly 500 medical practices in seven regions nationwide to help enhance care quality and reduce costs.
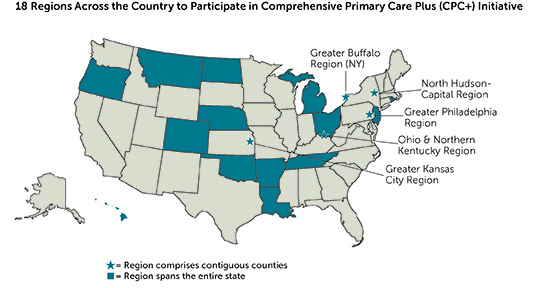
The release of Mathematica’s article and report comes as CMS has announced plans to launch Comprehensive Primary Care Plus, the next generation of its efforts to improve primary care. Mathematica’s findings on the second year of CPC, and its ongoing study of the initiative, will provide important evidence to inform policymakers and other stakeholders in U.S. health care reform.
In their study of CPC’s first two years, Mathematica researchers found the strongest improvements in care management for high-risk patients and in access to care. However, the estimated reductions in Medicare expenditures resulting from the CPC initiative were not enough to offset the fees that Medicare provided to participating practices.
"Transforming primary care is difficult work, but these practices have made headway," said Stacy Dale, a senior researcher at Mathematica and lead author of the article in the New England Journal of Medicine. "The CPC effort has provided substantial financial resources, technical assistance, and performance feedback to support these transformations. After only two years, it is promising that CPC seems to be having a small favorable effect on Medicare expenditures, but going forward the effect will have to be substantially larger to cover the costs of the initiative."
A large body of research has shown that patients often do not receive well-coordinated care, leading to duplicative or ineffective treatment, excessive costs, and poor outcomes. The CPC initiative focuses on primary care practices because patients typically see these doctors first when symptoms arise and rely on them to manage the bulk of their care, make referrals to specialists when needed, and coordinate the care they receive from other providers.
The CPC initiative requires that participating practices meet annual milestones that help them improve their performance in five key areas: access and continuity, planned chronic and preventive care, risk-stratified care management, patient and caregiver engagement, and coordination of care with other medical providers.
Based on survey data collected by Mathematica, risk-stratified care management was the area of greatest improvement over CPC’s first two years. Practices took a more proactive approach to care by assessing each patient’s risk of future health problems. They then delivered more proactive care to high-risk patients through efforts such as assigning nurse care managers to follow up with patients during or after a hospital stay to try to reduce preventable readmissions, and working with patients who have chronic conditions to improve their self-care and medication management.
Participating practices also improved access to care through efforts such as expanding same-day appointments, reducing waiting times, and establishing online portals to let patients obtain health information, Mathematica found.
Deborah Peikes, a Mathematica senior fellow and the principal investigator of the CPC study, noted that the nearly 500 participating practices are diverse and include nearly 2,200 clinicians in small and large practices, physician- and system-owned practices, rural and urban practices, and primary care and multispecialty practices. Given the scope of the effort, Mathematica’s ongoing study will be of interest to many stakeholders involved in U.S. health care reform, she said.
"We will continue to learn more about patient experience, costs, service use, care quality measures, and clinician and staff satisfaction with the initiative," Peikes said. “Our goal is to understand how specific changes in how practices deliver primary care can affect outcomes to guide future efforts to improve care delivery. Our initial assessment of this linkage shows that practices making the largest overall improvement in care delivery have substantially greater reductions in hospitalizations, on average. Our future efforts will attempt to measure which specific types of enhancements are associated with the greatest improvements in costs and quality of care, and how that relationship differs across practices."
More information about Mathematica’s wide-ranging research on primary care reform and on Medicare is available on our website.