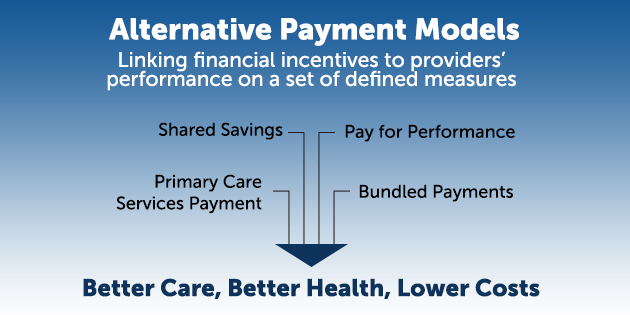
Federal agencies such as the Centers for Medicare & Medicaid Services (CMS)—particularly its Center for Medicare & Medicaid Innovation—have invested significant resources in the move from traditional fee-for-service payment to alternative payment models that reward efficient, high quality, and patient-centered care. This shift often requires substantial policy, structural, and operational changes at every level of service delivery. Yet evidence is available to help policymakers and leaders of health care systems and programs leverage the potential of payment reform to improve health care and outcomes while reducing costs.
In Mathematica’s new issue brief, “Developing Alternative Payment Models: Key Considerations and lessons Learned from Years of Collaboration with CMS,” our health policy experts review the important issues that can arise in designing, implementing, monitoring, and evaluating alternative payment models. The brief gives decision makers the guidance they need to address these issues so they can improve service quality, control costs, and meet providers’ and patients’ needs with flexible care. Topics covered in the brief include:
- The design and implementation of payment reforms
- The evaluation of primary care practices and payment reforms
- The support available for providers who use the alternative payment models
Read the brief and the companion fact sheet.