Swept into the whirlwind of the congressional debate this year on changes to the Affordable Care Act were proposals to reform the Medicaid program. Medicaid is now the most common type of health insurance, covering 70 million Americans in 2015 (up from 46 million in 2005) and has attracted the attention of reformers because of its cost. Although the growth of Medicaid’s per capita cost over the past decade falls below that of Medicare and private payers, the large increase in the number of people covered by Medicaid pushed total program spending to over $556 billion in 2015.
At the same time, Medicaid coverage doesn’t necessarily guarantee access to care. An estimated 30 percent of all physicians in 2013 said they did not accept new Medicaid patients, an often-mentioned—and widely debated—issue in the discussion of health care reform.
Federal and state Medicaid officials recognize that just having a Medicaid card alone does not guarantee timely access to primary care, specialty care, obstetric and neonatal care, behavioral health services, and other essential benefits. For that reason, these officials have jointly devised policies and oversight practices to ensure that Medicaid beneficiaries get the right care at the right time from providers in their communities or within a reasonable distance.
In 2016, the federal government updated the rules that set minimum standards for the availability of both services and providers for the 75 percent of Medicaid beneficiaries who receive their care through managed care plans. Just like the federal rules dating back to 2002, the 2016 regulations require states to ensure that managed care plans have enough providers in their networks to assure adequate access to covered services. But the 2016 rule also clarified that states should achieve that objective by (1) creating standards for provider networks based on reasonable travel time and distance between beneficiaries’ homes and providers’ offices, (2) developing systems and metrics for monitoring access to care, and (3) considering the special needs of people with disabilities who are increasingly enrolled in managed care plans.
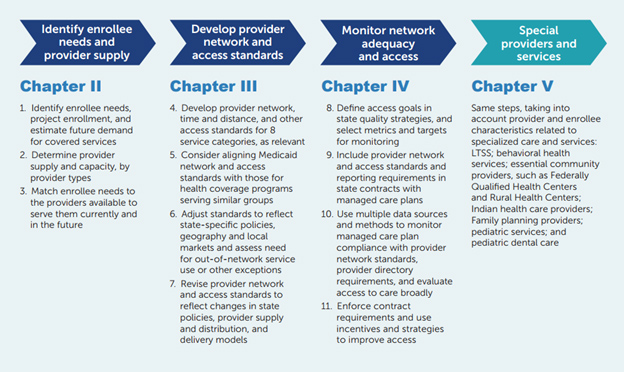
To help state officials meet these requirements, the Centers for Medicare & Medicaid Services asked Mathematica to create a guide that covers information, resources and exemplary state practices. Released this past summer, the toolkit is designed to help states develop standards for adequate networks and available services for Medicaid and Children’s Health Insurance Program (CHIP) managed care plans. The toolkit also offers a framework and suggested metrics for monitoring the availability of services, the adequacy of provider networks, and broader indicators of access to care. Developed in partnership with the National Association of Medicaid Directors and dozens of state Medicaid officials, the toolkit features strategies and techniques that can be easily replicated in, or customized to, each state to meet the needs of beneficiaries of all ages who have myriad health conditions and types of disabilities, and who live in a variety of geographic areas.
Promoting Access and Ensuring Provider Network Adequacy and Service Availability in Medicaid and CHIP Managed Care Programs
While federal and state policymakers debate broader or long-term reforms to reduce the cost of Medicaid and improve its outcomes, state Medicaid agencies can take steps now to improve access to care. Using the toolkit as a guide, they can work closely with managed care plans, providers, and consumers to make sure that Medicaid coverage isn’t just a card. If state Medicaid agencies establish well-designed network standards, and if they use strong oversight systems, the Medicaid card that millions of beneficiaries keep in their wallets can become their passport to timely and essential medical, behavioral, and long-term services and supports.


