When I worked for Maryland’s health department as its chief of health information technology policy for four years, I helped the state rethink its approach to measuring the quality and outcomes of health care—particularly in relation to leveraging new data sources. Like many states, Maryland has taken important steps toward reforming health care payment and delivery. Thinking through how to measure quality is always a complicated yet essential part of making and monitoring changes to payment and delivery systems.
Since joining Mathematica last year, I have been thinking about how health care insurers—be they federal or state government agencies or private insurers—can make the shift from assessing doctors based mainly on the kind or volume of services they provide (process measures) to assessing them based on the value of care, including the health and well-being of patients after they receive services (outcome measures). I am increasingly convinced that, before we can pay clinical teams for improving our health, we need better ways of measuring the impact of their services.
Given the technological improvements made in the last decade, it’s now time to revisit what’s possible in terms of measuring and promoting good performance in health care. From Alex Azar, secretary of the U.S. Department of Health and Human Services, to Atul Gawande, CEO of Haven (the new joint venture of Amazon, Berkshire, and JP Morgan Chase), a growing number of health care leaders in the public and private sectors are articulating the need and priorities for an outcomes-focused, value-based approach to performance measurement. We are brimming with data on health and health care experiences—including patient-reported outcomes and electronic health records—and have better tools for processing and interpreting those data than ever before. We can also receive these data in near-real time, and we have a growing body of evidence about how various payment models and performance feedback tools affect the behavior of clinicians and their teams. But we are all still figuring out how to effectively measure the value, rather than just the volume, of care.
Whether you’re a state health agency running a Medicaid program or a private payer designing an employer-sponsored plan, the best way to measure and reward value-based care will look different in each state and for each program. This variation depends on several factors, such as:
- The characteristics and needs of the beneficiaries
- The availability of data and the infrastructure used to collect and aggregate the data
- The resources available to clinicians, health care facilities, and program administrators
Process measures—particularly those that require new or different documentation—often place a heavy administrative burden on clinicians and their staff. Many health care leaders have called for replacing process measures with outcome measures so that all stakeholders can focus on the end goal: better health for patients, which would presumably come from high quality care and eventually result in lower costs. But in practice, most programs will need to measure a mix of processes and outcomes to encourage the use of the right care, at the right time and place, to meet each patient’s needs.
Selecting the right mix of process and outcome measures is no easy feat. Having seen the issues in play in Maryland, and now with a broader view from my seat at Mathematica, I created the following decision framework for public and private payers. This framework is designed to help payers select or update quality measures to better position themselves to set financial incentives.
Developing your approach to quality measurement
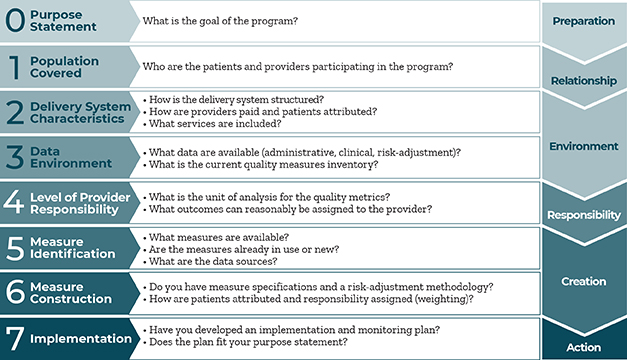
Broadly speaking, payers need to think about why it’s reasonable to assume that their program will affect the quality of care, whom to focus on, and where their program fits in the established environment before they can define what to measure, when to measure it, and how to operationalize that measurement approach.
It’s tempting to skip from identifying the population covered (Step 1) to selecting and creating measures (Steps 5 and 6), but the hard, meaningful work takes place between these two steps. For instance, carefully considering the current data environment (Step 3) allows for a more realistic assessment of which types of measures could be used and the options for connecting patients with the teams or facilities responsible for their care. Can you measure patient outcomes for individual clinicians, or would you need new or redesigned data collection systems? Are you and other stakeholders ready and able to make that investment? Thinking through these questions may identify areas where it’s not yet feasible to measure outcomes or where process measures would help you meet your program goals more effectively.
Skipping the intermediate steps also puts you at risk of missing the mark or introducing unintended consequences. If you create measure sets for programs without considering the characteristics of the delivery system (Step 2), achieving the desired outcomes may not be practical because of capacity constraints or barriers to access in your region. Similarly, asking clinicians and their teams to move the needle on outcomes that are affected by many factors outside of their control undermines their buy-in and, ultimately, your chances of success. Let’s be clear: process measures pose plenty of challenges, but in some cases, they may be the safer and more realistic option.
By sharing this framework, I hope to spark dialogue about how to select and update measure sets in value-based payment arrangements and other initiatives. For those of us who want to see the health care system adopt more outcome measures, we need to do it in a way that accounts for the needs and constraints of each place and program. These are some initial steps, but there is still plenty of work for us to do to create impactful and realistic value-based payment approaches.
If you have ideas about how to improve or expand on the framework, please email me at pmessino@mathematica-mpr.com.



